10 Principles of Patient-Centered Design

This blog was authored by Paul Chang, SVP, Design and Experience at Medidata.
In 2019, I had the privilege of working with Alicia Staley, patient advocate and three-time cancer survivor, to develop a workshop that would eventually evolve into the Medidata Patient Insights Board where she and our design team engage with patient advocates to gain insights on important patient-centered topics. Through these workshops, we’ve been able to appreciate the challenges that patients face with their healthcare journey and specifically when joining clinical trials.
Our childhood memories of jabs, pills, and procedures inform our visceral response to doctor’s visits. In the best case, we‘re going for a preventative checkup. In other cases, there’s a problem—and the visit can be stressful. Beyond medical visits, clinical trials present a lifeline when standards of care have proven inadequate. Some of us, like Alicia, have been through the process, while many of us know someone who’s reached this crossroad. Sometimes the outcome of a trial may not benefit them directly, yet they’re driven by the desire to help others who may follow. We hear stories and witness bravery, optimism, resilience—heroism.
The 10 principles of patient-centric design are for these heroes. These principles have been developed over five years of interactions with patients, patient advocates, healthcare professionals, and clinical trial administrators. They’re meant to guide contributors to the patient experience, and to be the calm in the chaos of each patient’s healthcare journey. We hope you find them useful.
1. Build Trust
Trust is a dynamic relationship. It’s tentatively granted, then tested over time. Manage patients’ expectations and perceived risks throughout their experience.
Transparency is often referenced as a key ingredient to trust-building and it’s no different here. Be open and honest about personal information and data sharing, potential conflicts of interest, and the risks and benefits of participation. Educate patients of anticipated burden—both financially and with respect to time commitment.
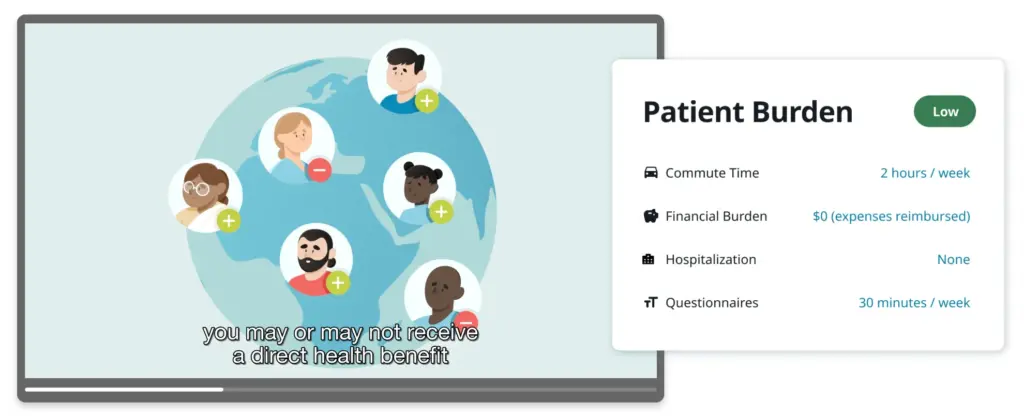
Build trust by providing easily scannable resources to help patients understand what they’re getting themselves into.
Build trust by opening channels for feedback and communication. This demonstrates a willingness and capacity to listen, learn, and support.
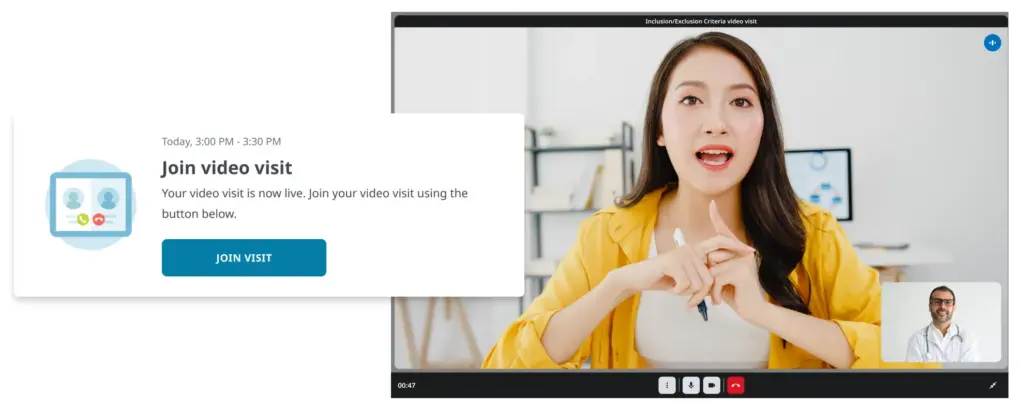
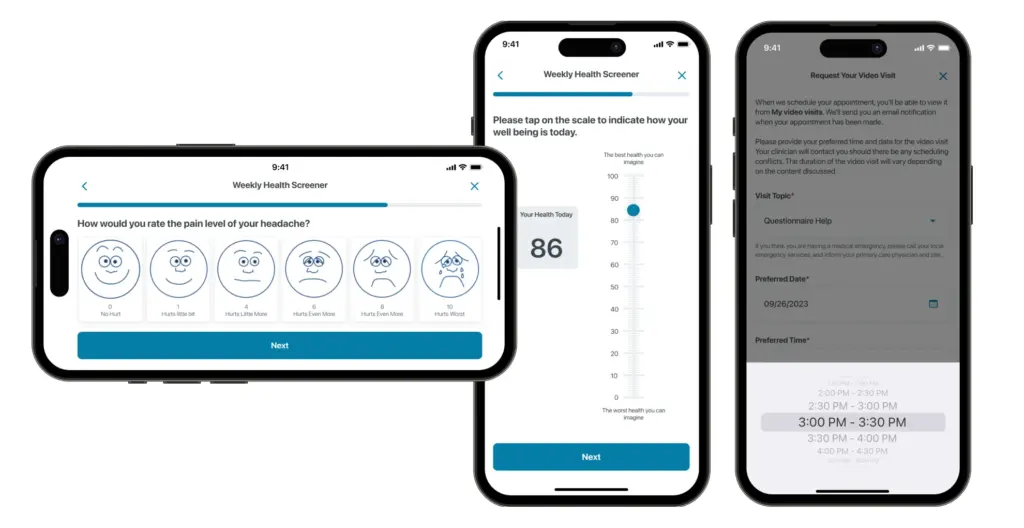
Regular patient connections with a clinician, whether through televisits or in-person visits, are crucial for building trust during clinical trials by fostering rapport and clear communication.
For a design deep dive, see how we create trust empathy maps to identify trust-building opportunities.
2. Develop a Good Bedside Manner
Put patients at the heart of everything you do. Make the patient feel cared for, comforted, and human before, during, and after their treatment or trial.
Start with a step-by-step agenda and provide the patient with a sense of place and time. This may seem elementary, but there are many examples where the patient is left to wonder “what’s next?” or “how much longer?”
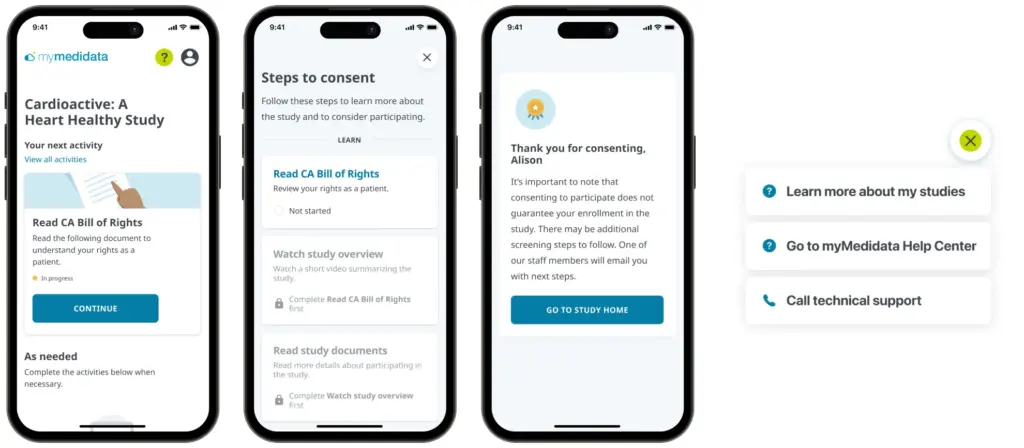
Inevitably, despite every effort to guide and nurture the patient through an experience, some will inevitably lose their way. In these cases, show the human on the other side by providing convenient help and support.
3. Be Inclusive
Good design is accessible to all.
Patient diversity is essential in developing meaningful outcomes in clinical and medical research because it ensures that findings are applicable across abilities, backgrounds, medical conditions, and cultures, leading to more accurate and effective healthcare interventions.

Be explicit about patient limitations supported (Source: Microsoft Inclusive Design).
4. Empower with Knowledge
Keep the patient informed and educated about their options so they can make good decisions.
Patients should be prepared to participate. This means providing educational resources during the decision-making process and at touchpoints throughout the process. And, don’t assume that the patient understands. Always confirm their understanding.
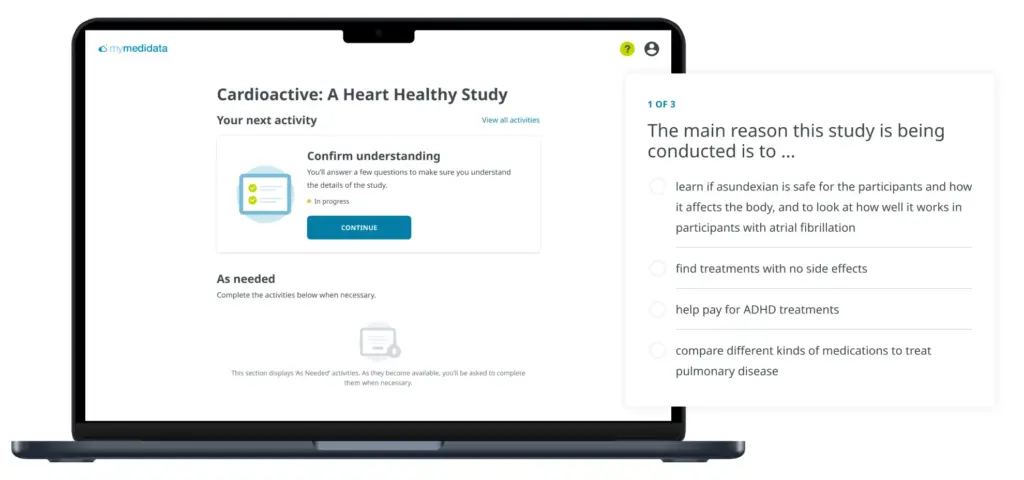
Provide a no-pressure comprehension checkpoint.
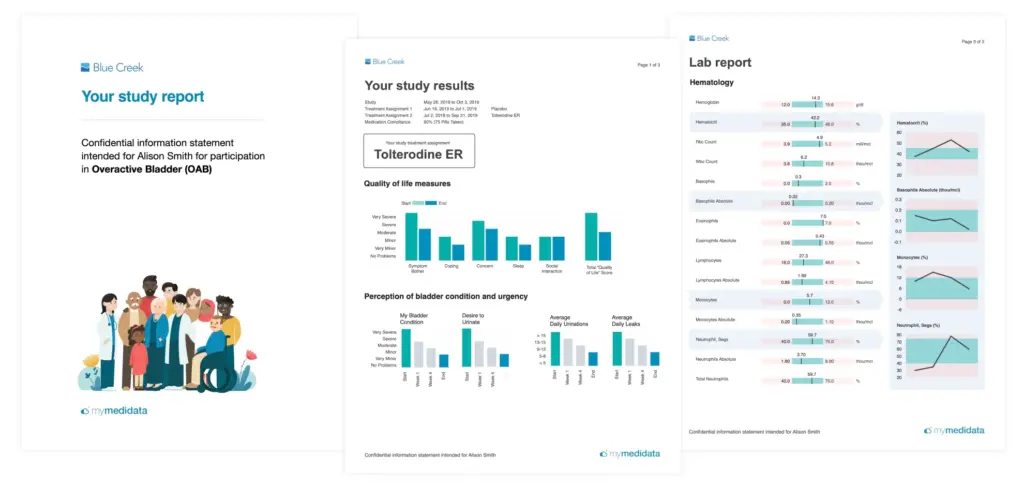
When the process or procedure is complete, be sure to share data back with the patient in a format that’s easy to understand and draw insights from, and that allows the patient to share data with selected family members, their primary care provider, and healthcare teams.
5. Give the Patient Control
Allow the patient to move at their own pace. Encourage interaction and dialogue, including feedback.
Empower patients to control their healthcare journey by providing them with flexibility to participate on their terms, choosing where, when, and how they engage. Allow adequate time for patients to ask questions and to make informed, shared decisions with their loved ones and healthcare team.
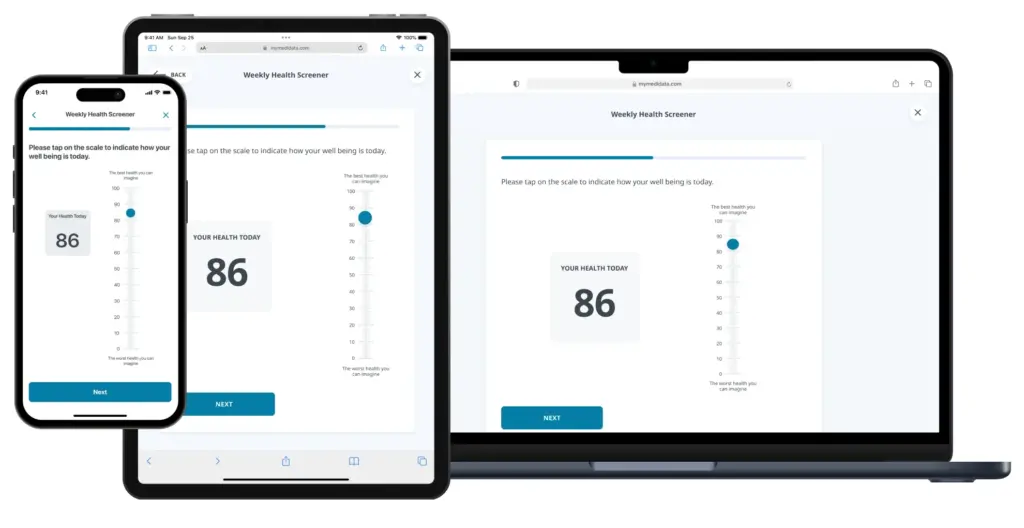
Embracing multi-channel access empowers users with flexibility, enabling them to engage with the experience on their own terms—whether through web, mobile, or other platforms.
6. Celebrate Wins
Acknowledge patient achievements and motivate their next steps.
When a process is completed, don’t just move on to the next task. Take the time to recognize each milestone in the process—high five! In gaming terminology, that’s called celebrating “win states.”
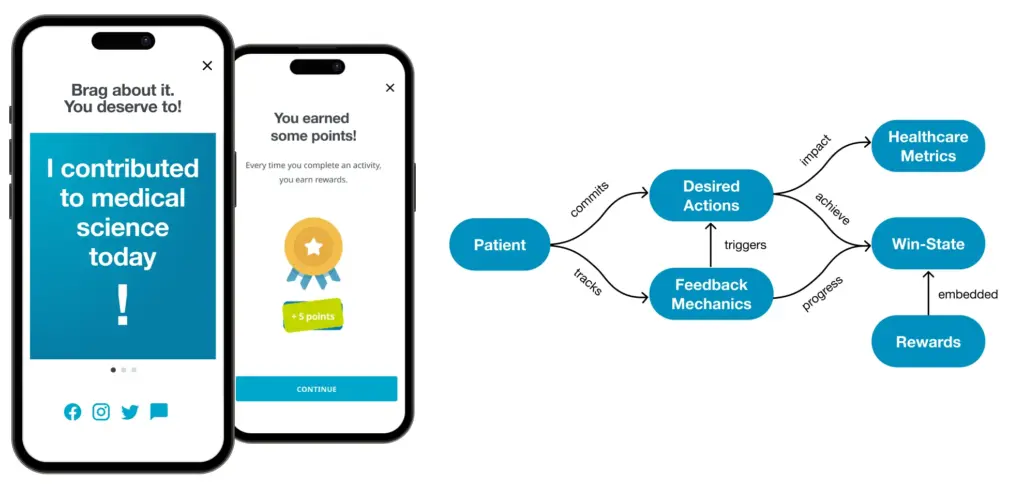
Celebrating accomplishments at various checkpoints throughout the patient’s journey is important as it acknowledges progress, boosts morale, and reinforces the significance of each milestone (win-state diagram source: Octalysis).
7. Don’t Make Them Think
Every element of a design should be in service of the intended patient action or outcome.
Reduce cognitive load whenever possible. While you may think a designed interaction makes perfectly good sense, it’s but one of many tasks in a patient’s busy day. They’re not reading, they’re scanning during a spare moment. Pursue simplicity relentlessly.
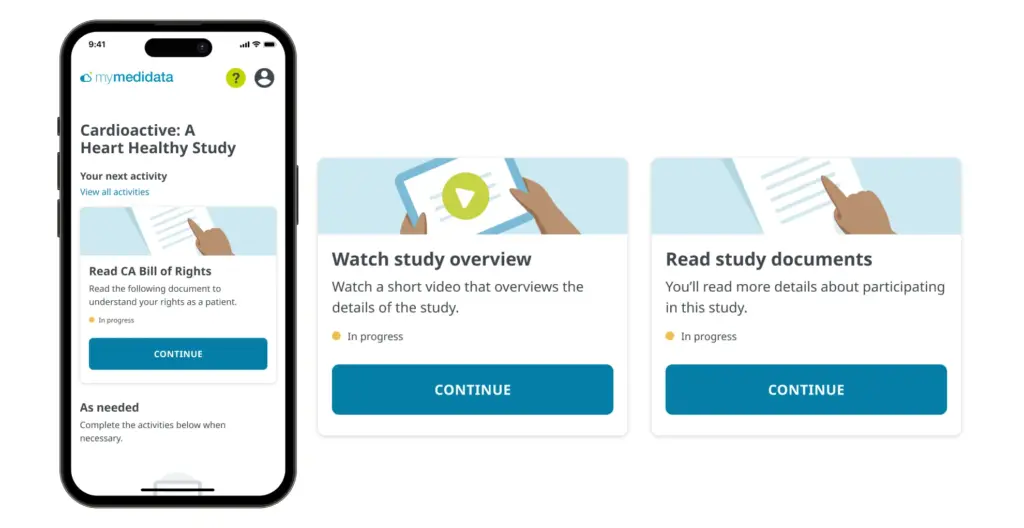
On the myMedidata platform, the patient experience has been distilled to a single “Next Activity” at any point in their clinical trial journey.
8. Don’t Reinvent the Wheel
When possible, use standard patterns and conventions.
Utilize familiar design patterns to tap into patients’ pre-existing mental models, offering a sense of comfort and ease of use. There are places to be creative, but navigation and typical computer interactions are not two of them.
On the other hand, intuitive patterns go beyond familiarity by anticipating patients’ needs and behaviors, often employing innovative or unconventional design solutions that feel natural and effortless.
Pay attention to when familiar will suffice and when non-standard yet intuitive designs are warranted.
Utilizing spatial and visual cues tailored to patients’ mental models enhances comprehension and interaction by providing intuitive pathways, fostering engagement, and reducing cognitive load.
9. Choose Words Carefully
Messaging and instructional content are critical to the patient experience.
Writing is often overlooked in the design process, yet it’s one of the most critical. It’s the aspect of our designs that patient advocates have commented on most often.
Speak in natural, non-technical language. Find the balance between casual, friendly language and a tone that respects context.
And, consider how certain words may fall upon patients’ ears. Historically, patients in clinical trials have been referred to as “subjects.” This terminology still exists and fails to acknowledge the patient’s voluntary role as a patient and partner in the process.
Am I data, or am I going to be seen as a real person?*
When I hear the word subject, I think of a criminal.*
I feel like one in a million, not one in a million.*
I think of an inanimate object—something that isn’t a person.*
*Quotes from Medidata Patient Insights Board members.
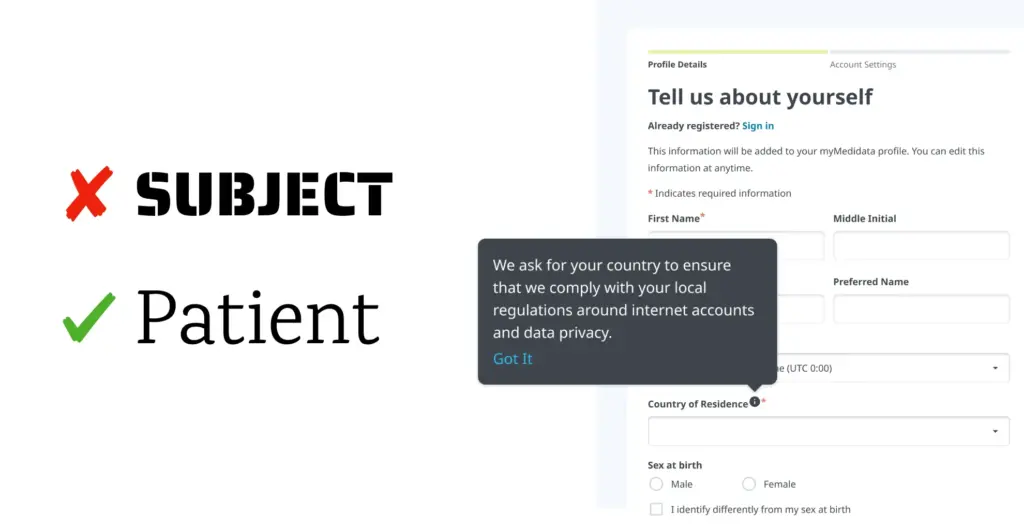
Friendly, human language goes a long way towards building trust and engagement.
10. Pay Attention to the Details
Proper typography and consistent design elements are critical to a trustworthy experience.
A consistently designed experience—from branding, to communication style, right down to font selection—all play a role in providing a trustworthy experience. Patients may enter the system from a variety of touchpoints (posts, e-mail, notifications, etc.) and you want them to know they’ve come to the right place.
Beyond consistency, quality is essential. If you don’t bother to dot your i’s and cross your t’s literally, what does that say for your healthcare practices?
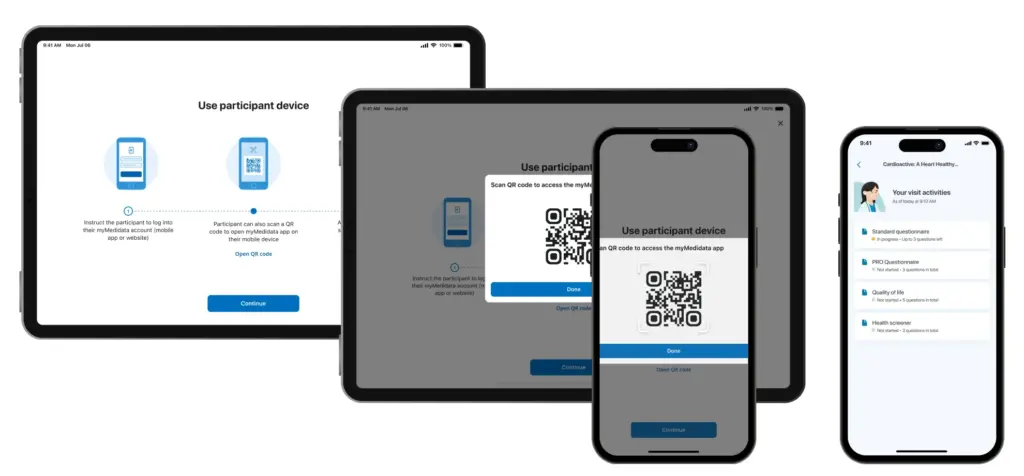
The design style changes in this handoff from clinician to patient, keeping the patient in an environment consistent with the rest of their experiences.
Final Thoughts
Patient-centered design is a powerful approach to improving the patient healthcare journey. Trust-building is the foundation on which all future interactions unfold. It’s built through transparency, listening, and learning—by showing that there are humans on the other side. From here, patient empowerment is constructed through knowledge and control, and only through inclusivity can we ensure better outcomes for all.
Acknowledgements
Special thanks to Alicia Staley and the Patient Insights Board at Medidata for their time, dedication, and inspiration; to Ben Berte and the Patient Cloud design team for their pursuit of better patient experiences, facilitation of patient-centered design workshops, and to Jesi Zhang for the design examples presented here. In memory of Linnea Olson and Sheila Johnson whose perspectives greatly influenced our understanding and development of these principles.
Contact Us
